A Medical and Health Insurance (MHI) policy is generally designed to cover the cost of private medical treatment, such as the cost of hospitalization and healthcare services, if you are diagnosed with covered illnesses or have had an accident.
The coverage is provided by a licensed insurance company, in exchange for which you pay premiums. Make sure that you deal only with a licensed insurance company or its authorized agents or a licensed insurance broker when you buy a MHI policy.
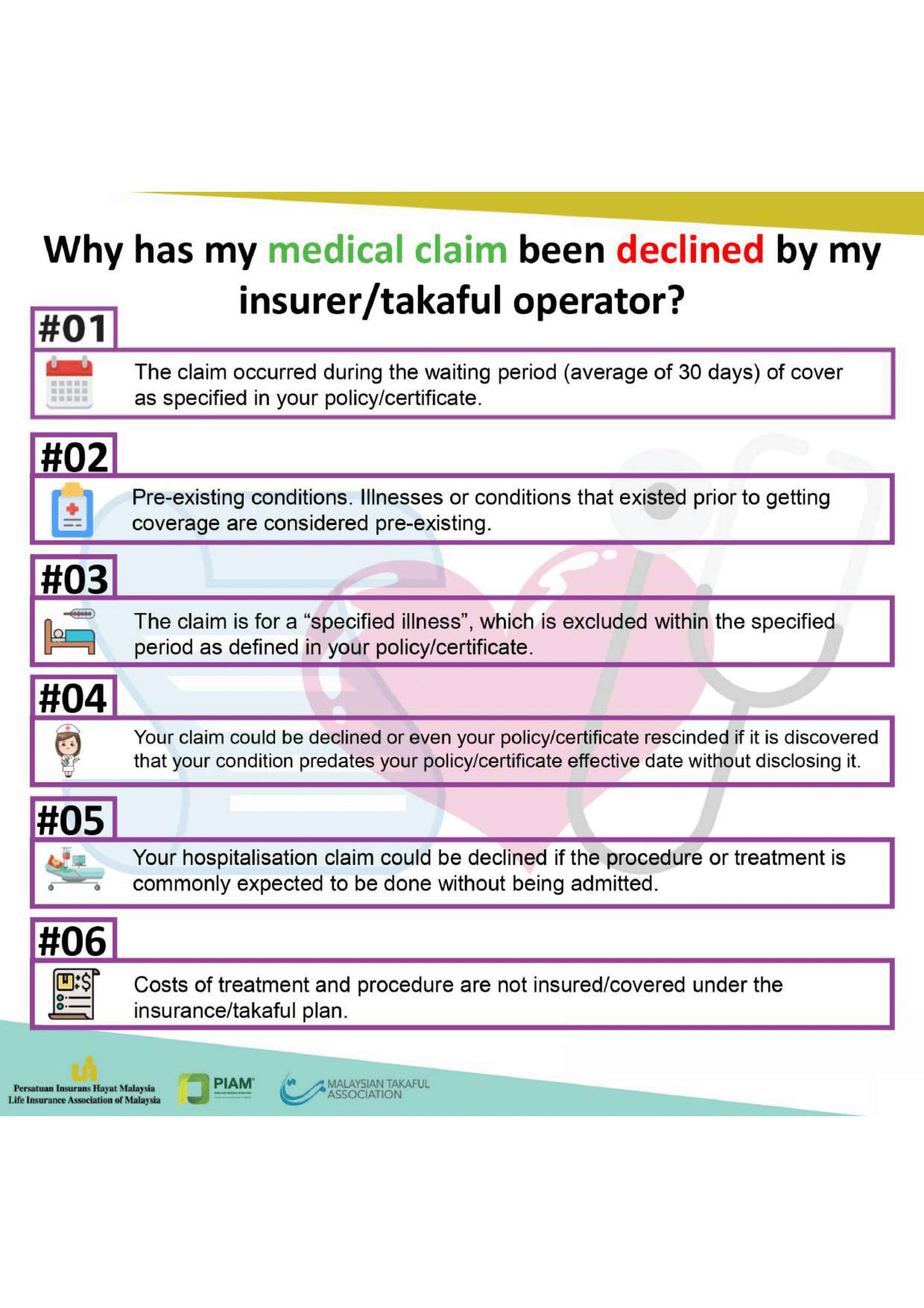
EXCLUSIONS
An MHI policy also contains certain exclusions, just like other insurance policies. You must be aware what these are and if you don’t understand them, ask your agent or insurance company. Some common exclusions are the following:
- Pre-existing conditions
Conditions and illnesses experienced by you prior to applying for the policy. These conditions and illnesses would be excluded from coverage by your insurance company. You should check with your insurance company regarding the details of pre-existing conditions for the policy that you intend to buy.
- Qualifying/waiting period
You will not be eligible for any claim arising from any medical or physical conditions within the first 30 days of the cover, except for accidental injuries.
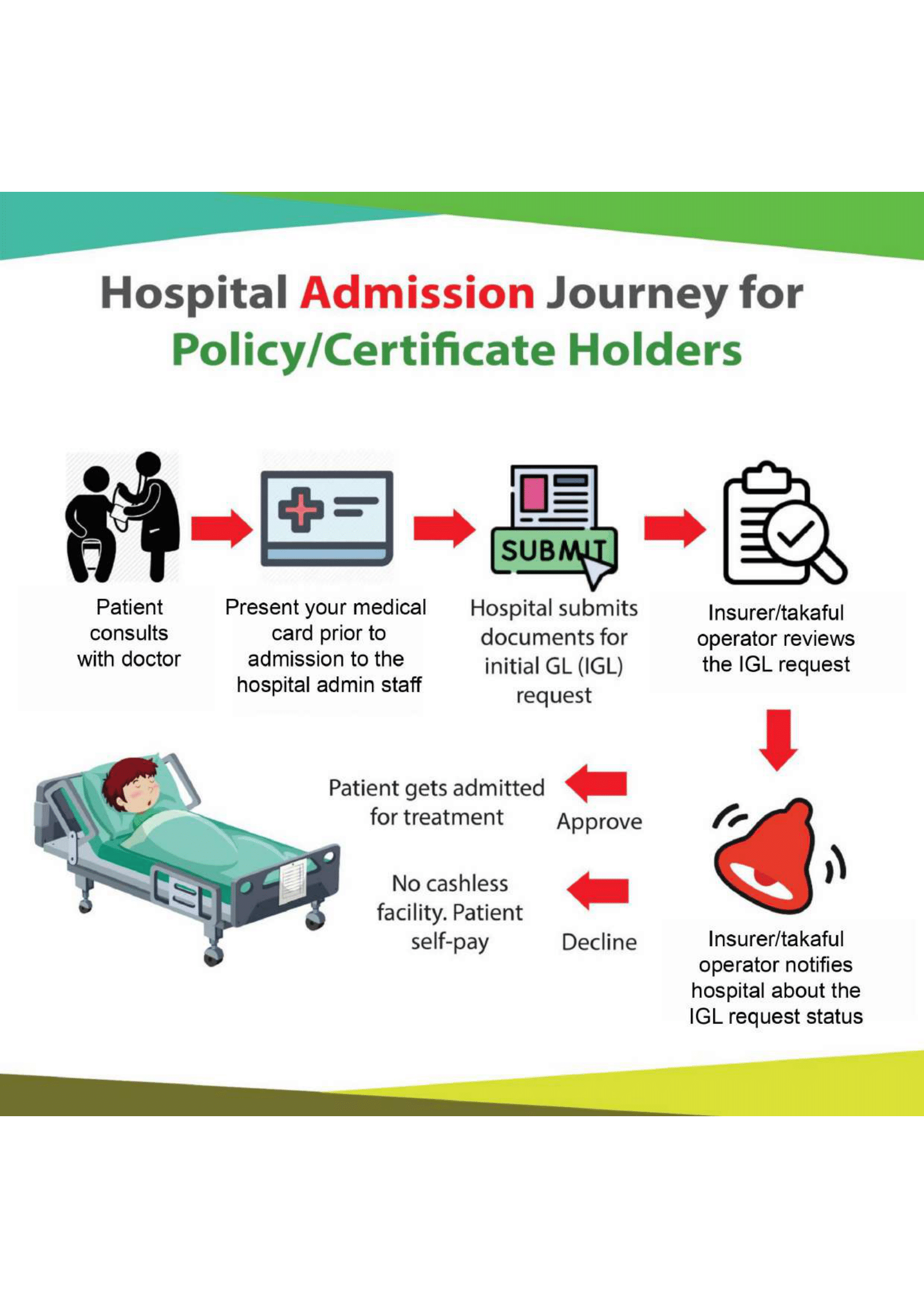
HOW TO MAKE A CLAIM
In order to minimize any unnecessary delays, the insurers advice that the following key actions are required as part of the claims process:
- Before receiving any non-emergency treatment, do call the customer care helpline of your insurance company or its third party administrator or your insurance agent to check whether your doctor’s proposed treatment is covered in your policy and whether your hospital of choice is part of the insurer’s panel of hospitals.
- Do request your doctor or specialist to fill in and sign your claim form. Your doctor may charge a small administration fee which may not be covered by your MHI policy.
- Do note that different insurers or different policy types offer different claim methods. Some insurers offer hospital guarantee letter issue service (cashless admission privilege) whilst others only reimburse hospitalization costs on receipt of original bills/receipts. Also the cashless admission privilege is only applicable for an insurer’s panel of hospitals/specialists. Non panel hospitals/specialists usually require the patient to settle the bill first then claim bill amount from their insurer.
- Do submit a written notice to your insurer as soon as possible, or within 30 days of the treatment period if you are diagnosed with a disability that would incur claimable expenses.
- Do send all claims documents together with the original bills and receipts, full doctor’s reports, physician’s cost summary of treatment and referral letter, if any.
More often than not, the payment process is slowed down or denied when the paperwork submitted is incomplete or supporting documents are missing. It is therefore important to check that all payment receipts, documents that require signatures are properly signed off and ensure that any other necessary reference material are attached as proof of treatment.
Do study your policy for any exclusion clauses. Please note that most MHI policies do not cover pre-existing conditions (i.e. medical conditions you had prior to the issuance of the policy). Other commonly excluded conditions include maternity related problems, congenital disorders etc. In the event that you require treatment for a condition that is not covered under your insurance plan, you may opt for treatment at a lower cost hospital. By knowing specifically what you are covered for would also save you the unnecessary hassle of submitting the paperwork for reimbursement and only to be denied payment later.